Mycology | Fungi of the skin. Do you know pityriasis versicolor?
Pityriasis versicolor
Bad call tinea versicolor. It is a superficial fungal infection of the stratum corneum of the skin, produced by lipophilic yeasts of the genus Malassezia, and is characterized by the appearance of hyperchromic, hypochromic or slightly pink spots or macules, of defined edges and irregular shape, which present a good desquamation. These injuries are mainly found in the trunk, neck, face and arms.

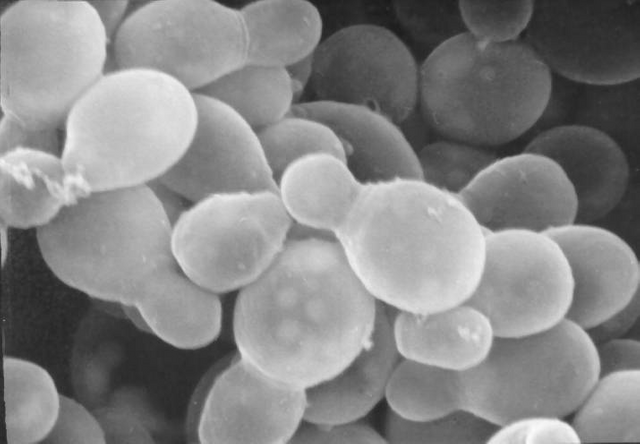
The causative agent is part of the human commensal microbiota and is located in the seborrheic areas of the skin. It does not discriminate age, sex and race. The fungus is transformed from commensal to pathogen under special conditions that allow the massive growth of blastoconidia and the production of hyphae.
The species of the genus have been recognized considering their morphological, physiological and molecular characteristics.
Species of the genus:
- Malassezia globosa
- M. furfur
- M. restricta
- M. sympodialis
- M. slooffiae
- M. obtusa
- M. pachydermatis
- M. nana
Otras...
Note: the first 5 species are responsible for Pityriasis versicolor. It is a cosmopolitan disease, which predominates in tropical climates.
Mycological diagnosis of pityriasis versicolor
For the mycological study of this condition, the following stages must be met:
- Clinical-epidemiological orientation.
- Fluorescence with wood lamp
- Sampling
- Direct examination
- Identification of the etiological agent.
Epidemiological clinical guide: In this stage, a diagnostic orientation is allowed, since depending on the clinical characteristics of the lesion, the study aims to identify the etiological agent. Likewise, the relevant epidemiological data or exclusion lead us to a more precise mycological study, such as age, sex, the recognition of predisposing factors, the time of evolution of the disease and others.
It should be noted that, in the case of using antifungals before the laboratory test, it may affect the chances of finding fungal elements in the parasitized tissues and the fluorescence in cases where it occurs, which will lead to a poor diagnosis, for therefore, the patient must return at least two weeks after the last treatment was applied.

Fluorescence in Wood's lamp: The patient is inspected with Wood's lamp, in a dark room, to detect the fluorescence of the lesions (lesions caused by Malassezia spp., Fluoresce yellow-ocher or yellow-green). Then, the lesions can be delimited by marking the edges with a ballpoint pen if necessary, to facilitate the location of the chosen sample. Fluorescence is not always observed, especially if it has been treated with antifungals, which does not rule out the diagnosis of pityriasis.
Clinical sample to select: Epidermal scales.
Sampling: the sample must be taken with the adhesive tape technique. To do this, cut a piece of clear adhesive tape that is slightly longer than the slide and place it over the chosen lesion with the adhesive part, press hard (without using the nail) and remove it vigorously. The lesion should be traced on the adhesive tape, stretched and placed on clean slides without exerting pressure, bending the ends towards the bottom of the sheet. This technique is the one of choice since it is easy and allows to keep together so many fungal structures to observe them under a microscope without producing a dispersion due to the mounting liquid.
In the absence of the tape, the lesion can be scraped with a sterile scalpel and the epidermal scales collected between two previously flamed sheets or also in a sterile petri dish. Another technique that can be used is to scrape the lesion with a sterile blade.
Direct examination: The clinical sample can be observed under the microscope by adding:
- Lightening liquid (KOH or 10% NaOH).
- Lightening liquid (10% KOH) and a drop of Parker blue black ink to stain the fungal structures.
- Diluted methylene blue
Note: the mounting liquid is placed by capillarity through the edges of the adhesive tape containing the sample.
Findings: blastoconidia of 3 to 8 μm are observed, with unipolar budding and thick refractive wall with marked tendency to occur in accumulations and associated with hyaline hyphae of 2.5 to 4 μm in diameter, short, thick and little branched.
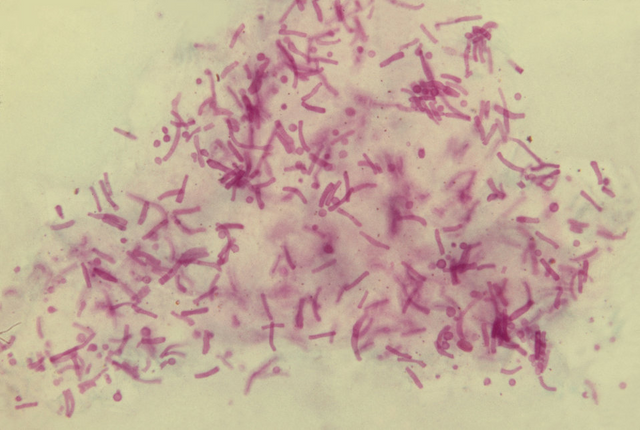
With these findings the diagnosis of pityriasis versicolor is established, although cultivation and molecular biology can be carried out for epidemiological and research purposes, the direct examination is based on laboratory diagnosis.
Mode of notification: blastoconidia and short hyaline hyphae compatible with Malassezia sp.
Treatment: a capsule of ketoconazole in the morning with a juice of naraja or commercial shampoo with antifungal .
In more severe cases: In general apply lotions, foams, creams or soaps with salicylic acid or sulfur at 1 to 3%, iodized solutions at 1%, others, which should be applied for a maximum of 15 minutes to avoid adverse effects to the components. It has been shown that changing the tropical climate to cold weather improves injuries.

.png)
Bibliographic references:
- Bonifaz JA. Micología Médica Básica: micosis superficiales y pseudomicosis superficiales, Pitiriasis versicolor e infecciones por Malassezia spp. 4ta ed. México: McGraw-Hill. c2012. p. 135-141
- Arenas R. Micología Medica Ilustrada: micosis superficiales, Pitiriasis versicolor. 5ta ed. México: McGraw-Hill. c2014. p. 99-111
Very good scientific work. How can you protect yourself or, if a person is infected with pityriasis versicolor, which medicine or natural can help against it?
I use Ore'gano oil to prevent yeast fungi! Alternatively, MMS can certainly help.
An upvote from me. Follow me on my blog :)
Thanks friend. There are people who have much easier to get the infection by various factors such as the amount of the microorganism, the production of fats, sweating, hot climates. This fungus is part of the normal flora of the skin, so it is important to have clean and dry skin. Sweat and hot climates favor the reproduction of the microorganism since it is lipophilic (it likes fats). A home medicine is not available, but a single dose of a ketoconazole pill in the morning with an orange juice is effective. In more severe cases medical treatment.